Concussions Forms & Policies
-
If your child has sustained a suspected concussion, the athletic trainer and/or coach at your athlete’s school will provide you with further medical instruction, which could include immediate transportation to the ER. Before your child can return to play, he/she must have a written medical release from the student’s licensed healthcare provider and the athletic trainer at the athlete’s school. An information sheet will be provided to you, as will our return to play guidelines. For more information or educational resources, please contact the Athletic Department or the Certified Athletic Trainer at your athlete’s school.
-
What is a concussion?
A concussion is an injury to the brain that temporarily changes how the brain normally works. It is usually caused by a direct blow or jolt to the head, face, or body with an “impulsive force” transmitted to the head. Signs and symptoms of a concussion can include dizziness, headache, vomiting, confusion, acting dazed, forgetting what happened before or after the injury, and/or loss of consciousness. A person does NOT need to be “knocked out” or lose consciousness to have a concussion. Other words or terms for a concussion include mild traumatic brain injury (mild TBI) and mild closed-head injury.What are the possible long-term effects of a concussion?
There is a possibility of long-term effects on a person’s health when a concussion is sustained. These effects can include Post-concussion syndrome, Dementia Pugilistica, and the possibility that the affected person may suffer from cumulative effects of multiple concussions. In Post-concussion syndrome, symptoms do not resolve for weeks, months, or years after a concussion, and may occasionally be permanent. Symptoms may include headaches, dizziness, fatigue, anxiety, memory and attention problems, sleep problems, and irritability. Dementia Pugilistica, or chronic encephalopathy, is an example of the cumulative damage that can occur as the result of multiple concussions or less severe blows to the head. The condition can result in cognitive and physical deficits such as Parkinsonism, speech and memory problems, slowed mental processing, tremor, and inappropriate behavior. It shares features with Alzheimer's disease. Cumulative effects may include psychiatric disorders and loss of long- term memory. Three or more concussions are also associated with a fivefold greater chance of developingAlzheimer's disease earlier and a threefold greater chance of developing memory deficits. After the initial concussion, there is a period in which the brain is particularly vulnerable to further injury. If an athlete sustains a second concussion during this period, the risk of permanent brain injury increases significantly and the consequences of a seemingly mild second concussion can be very severe, and even result in death (i.e., “second impact syndrome”).
-
What are the possible short-term effects of concussions?
Most young people will recover completely from a single concussion within one to two weeks. However, some people can take longer to recover than others. Common problems seen after a concussion are listed below. You should watch for these problems. Talk with your child’s licensed healthcare provider about any changes that you notice in these areas:- Physical:
Headaches
Sick to Stomach
Dizziness
Low Energy Level
Trouble with Vision
Bothered By Light
Sleeping Problems - Thinking (Cognitive)
Slowed Thinking
Trouble Paying Attention"Difficulty Remembering
Acting in a "Fog"
Easily Confused
School Performance Suffers - Behavioral or Emotional
Irritability or Grouchiness
Easily Upset/Frustrated
Nervousness
Sadness
Acting Without Thinking
Personality Changes
Please note that with a concussion your child may only display one of the above symptoms or a combination of symptoms.
- Physical:
-
Concussion Policy
The following policy was developed to provide general guidelines for the management of concussions in athletes. The Sentara Sports Medicine Department has created this action plan to educate athletic trainers, coaches, athletes, and parents on the proper management and referral process for individuals who may sustain a concussion during competition. The policy has been established based on the current literature from the National Athletic Trainer’s Association (NATA), Korey Stringer Institute (KSI), and Virginia Law.
Sentara Concussion Policy _pdf
Definition:
A concussion is a traumatic brain injury and is defined by the 4th International Conference on Concussion in Sports (2012) as a complex pathophysiological process affecting the brain and induced by biomechanical forces. Several common features that incorporate clinical, pathologic, and biomechanical injury constructs that may be utilized in defining the nature of a concussive head injury include the following:- Concussion may be caused either by a direct blow to the head, face, neck, or elsewhere on the body with an "impulsive" force transmitted to the head.
- Concussion typically results in the rapid onset of short-lived impairment of neurologic function that resolves spontaneously. However, in some cases, symptoms and signs may evolve over a number of minutes, hours, or days.
- Concussion may result in neuropathological changes, but the acute clinical symptoms largely reflect a functional disturbance rather than a structural injury with no abnormality seen on standard structural neuroimaging studies.
- Concussion results in a graded set of clinical symptoms that may or may not involve loss of consciousness. Resolution of the clinical and cognitive symptoms typically follows a sequential course. It is important to note, however, that symptoms may be prolonged in some cases.
-
Concussion Graduated Return to Play
When an athlete has been evaluated by an athletic trainer and/or a physician for a concussion, the following graduated functional return to play will be followed. The return to play progression will not begin until the athlete is completely symptom free. Each step is a 24-hour period; therefore, the return to play progression will be a minimum of 6 days. If the athlete experiences any symptoms, at any point during the rehabilitation steps, the progression will stop immediately, and the cycle will resume at the previous asymptomatic rehabilitation step after 24 hours of rest. If symptoms continue to occur for 2 consecutive days, the athlete will be referred back to the physician
for a follow up evaluation. When the athlete has successfully completed Step 4 (Non-Contact Drills) of the progression, they will be IMPACT tested using the computerized neuropsychological testing battery to help assist in a safe return to play. The IMPACT results will be reviewed by the physician and return to play status will be determined at this point. Please note that the IMPACT test results will not be the sole determining factor for return to play.
*Adapted from Table 1 McCrory et al. Consensus Statement on Concussion in Sport 3rd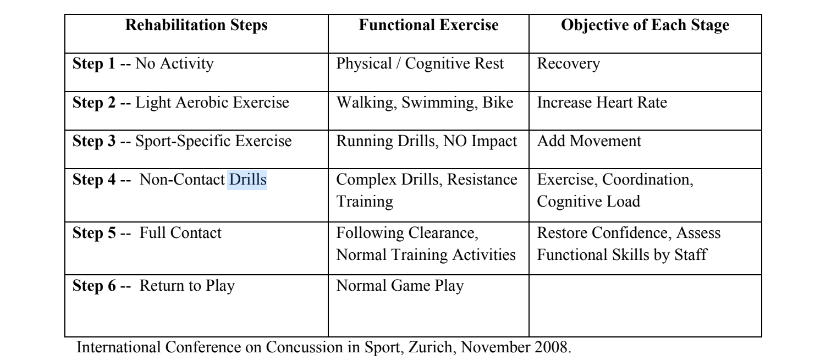
International Conference on Concussion in Sport, Zurich, November 2008. The treatment, management, and return to play determinations will be individualized to each athlete and dependent on circumstances of each specific case and injury. A safe return to play is the ultimate goal regardless of age and level of play. For more information regarding concussion, please visit the following websites:
http://www.cdc.gov/concussion/HeadsUp/high_school.html
https://www.vhsl.org/sports-medicine-links/
www.nata.org

